Fracture
Fracture Management
Fracture management focuses on achieving anatomical and functional alignment. This is achieved in different ways depending on the fracture:
- bracing and casting are used for non-displaced / minimally displaced fractures

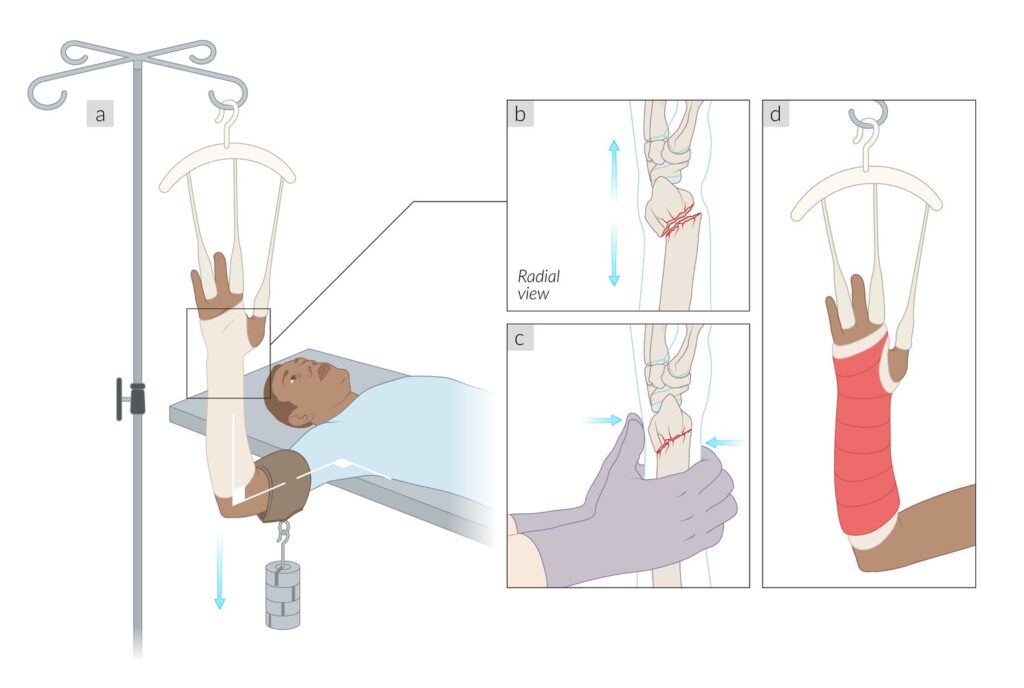
- reduction and immobilisation are used for displaced fractures
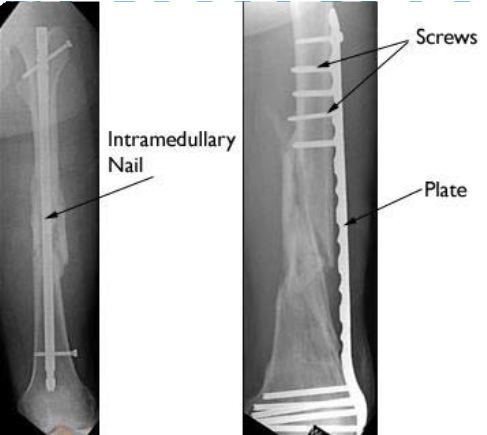
- surgical stabilisation is typically required for displaced, unstable fractures – this often involves open reduction (surgical realignment) and internal fixation (e.g., plates, screws, rods)
Fracture management will depend on many different factors, including the type and severity of a fracture, how it has been fixed, the stability of the fracture, individual factors, the stage of healing, etc. Depending on the injury, the physiotherapy and rehabilitation management may focus on the following aspects.
Initial phase (immobilisation / early healing): during the initial phase, treatment focuses on pain management and swelling reduction while maintaining the mobility of joints above and below the fracture. This phase also includes patient education on weight-bearing status, necessary precautions, and techniques for safe transfers and movements.
Post-immobilisation (after the cast or brace is removed): the post-immobilisation phase concentrates on restoring range of motion while implementing progressive strengthening exercises and functional rehabilitation techniques. During this period, scar management is also addressed to promote optimal healing and minimise tissue restrictions.
Advanced rehabilitation: involves progressive strengthening exercises complemented by balance and proprioception training, as well as gait re-training to restore normal walking patterns. This phase focuses on facilitating the patient’s return to work, sport, and activities of daily living while addressing any identified deficits that may impact functional performance.